Abstract
BACKGROUND: Patients with preoperative anemia are at increased risk of postoperative blood transfusion, as well as other adverse outcomes, including infection, prolonged length of stay (LOS), and death. Requirement of intraoperative transfusions may be an independent risk factor for mortality among patients undergoing noncardiac surgery. As such, efforts have emerged internationally to establish clinical decision support tools, dedicated preoperative anemia clinics, and clinical trials studying the effects of preoperative treatment of patients to improve outcomes after surgery. While studies to date have shown mixed results, some suggest that treatment with intravenous (IV) iron improves anemia and decreases transfusion requirements. Treatment with erythropoietin-stimulating agents (ESA) has also been associated with fewer transfusions in patients undergoing orthopedic surgery.
METHODS: We established a preoperative clinic in 2019 with a pilot for patients undergoing spine surgery. Patients who were found to have a hemoglobin (Hgb) < 13.0 g/dL on preadmission testing were automatically referred, and when possible, had iron studies reflexively added on to their samples. Patients were offered an appointment with a nurse practitioner or physician in Hematology and treated with IV iron or a combination of IV iron and ESA at the discretion of the provider. Importantly, if time did not allow for a visit or the patient declined an appointment or preoperative treatment, surgeries were not cancelled or delayed.
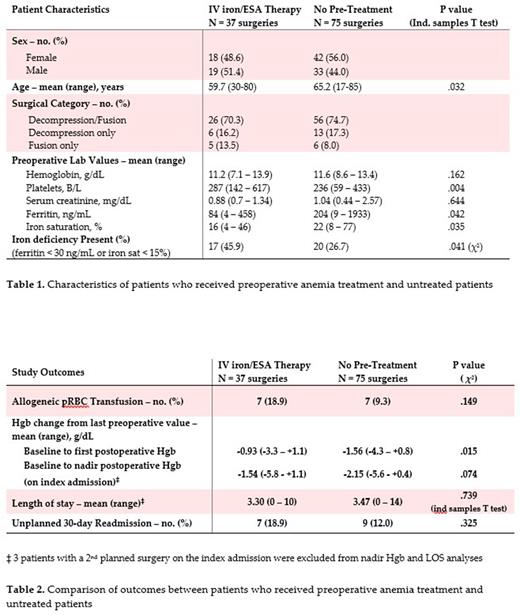
This retrospective study included patients undergoing elective spine surgeries between August 1, 2019 and June 1, 2021 at Thomas Jefferson University Hospital and Jefferson Hospital for Neuroscience. Patients were eligible if they were automatically referred to the preoperative anemia clinic based on preadmission testing results. The primary outcome was postoperative allogeneic red blood cell (RBC) transfusion during the index admission. Secondary outcomes included decrease in Hgb postoperatively, LOS, and 30-day readmission rate.
RESULTS: The study included 108 patients (53.7% female) who underwent a total of 112 distinct elective spine surgeries. The median age at the time of surgery was 65 years. The most common surgery was decompression and fusion (73.2%), followed by decompression (17.0%) and fusion (9.8%). 16.1% of surgeries were revisions of a prior surgery. The median preoperative Hgb was 11.6 g/dL.
Prior to the 112 surgeries, 45 (40.2%) patients were seen by a Hematology provider and 37 (33.0%) received preoperative treatment for anemia, including 28 (25.0%) who got IV iron plus ESA, 8 (7.1%) IV iron alone, and 1 (0.9%) ESA alone. The final treatment was given a median of 5 days before surgery (IQR 3-9.5 days). There was a nonsignificant trend toward lower mean preoperative Hgb in patients who were treated before surgery and those who were not (mean 11.2 vs 11.6 g/dL, p=.162) and greater mean estimated blood loss during surgery when reported (392 vs 315 mL, p=.462). Compared to untreated patients, those who were treated before surgery were significantly more likely to be iron deficient (ferritin < 30 ng/mL or iron saturation < 15%) (45.9% vs 26.7%, p=.041).
The primary outcome of allogeneic RBC transfusion occurred in 18.9% of patients who received pre-treatment and 9.3% of those who did not (p=.149). The degree of initial Hgb drop postoperatively from last pre-op value was significantly lesser in pre-treated patients (-0.93 vs -1.56 g/dL, p=.015), and a nonsignificant improvement was observed in the change from baseline to nadir Hgb during the index admission (-1.54 vs -2.15 g/dL, p=.074). A trend toward shorter LOS was observed in pre-treated patients (3.30 vs 3.47 days, p=.739), though that group also experienced more 30-day inpatient readmissions (18.9 vs 12.0%, p=.325). No deaths were observed during the study period.
CONCLUSION: In this preoperative anemia clinic pilot, treatment with IV iron and/or ESA before major spine surgery was not associated with a reduction in allogeneic RBC transfusions or hospital readmission. However, those who received pre-treatment had significantly lesser declines in Hgb after surgery and a trend toward shorter LOS. Patients who received treatment were significantly more likely to be iron deficient before surgery and had lower mean Hgb levels, which confounds the results. Larger prospective studies of preoperative anemia therapy are needed.
Disclosures
No relevant conflicts of interest to declare.
OffLabel Disclosure:
Our study includes patients treated with off-label intravenous iron before elective noncardiac surgery
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal